Please add me to your newsletter and send me more info!
It happens when the pancreas does not make enough insulin or when the body cannot use insulin effectively.When this system doesn’t work, sugar builds up in the blood instead of being used for energy. No matter the type, diabetes can strain the body over time and lead to serious health problems if left unmanaged.
Over time, that can cause serious health problems, such as heart disease, vision loss, and kidney disease.1
● When insulin works well: Your muscles, fat, and liver cells get the fuel they need, and blood sugar levels stay balanced.
● When insulin doesn’t work properly (insulin resistance or lack of insulin):
- Glucose builds up in the blood (high blood sugar).
- Cells starve for energy even though sugar is available.
- Over time, high blood sugar damages blood vessels and nerves, leading to complications such as heart disease, kidney problems, and vision loss.
Insulin is not just about numbers on a glucose meter, it’s what keeps your body’s energy system running smoothly and protects long-term health.
There are several categories of diabetes, each with different causes and management needs:
It can appear at any age, though it is most common in children and young adults. People living with type 1 diabetes need daily insulin injections, regular blood glucose monitoring, and a healthy lifestyle to manage their condition effectively. While the exact cause is still unknown, having a close family member with type 1 slightly raises the risk. Environmental factors, like viral infections, may also trigger the autoimmune reaction.
Currently, type 1 diabetes cannot be prevented or cured—management focuses on insulin therapy along with blood glucose monitoring and healthy daily habits.2
Type 2 diabetes is the most commonly diagnosed type of diabetes, making up over 90% of all cases. It develops when the body does not respond properly to insulin (insulin resistance), often combined with reduced insulin production over time. At first, the pancreas produces extra insulin to compensate, but eventually it cannot keep up leading to rising blood glucose levels (hyperglycemia).
While it mainly affects older adults, increasing rates of obesity, physical inactivity, and poor diet have led to rising cases in younger people, including children and adolescents. Family history also raises the risk.
Managing type 2 diabetes often starts with a healthy diet, regular physical activity, not smoking, and maintaining a healthy weight. Many people also require oral medications and sometimes insulin to help control blood glucose.
With prediabetes, the body’s cells don’t respond properly to insulin. Prediabetes can go unnoticed for years because there are often no symptoms. Many people only find out once other health problems develop.
You may be at higher risk if you are overweight, over 45, have a parent or sibling with type 2 diabetes, are physically inactive, or have a history of gestational diabetes. Some racial and ethnic groups—including African American, Hispanic/Latino, Native American, Pacific Islander, and some Asian communities are also at higher risk.The good news: lifestyle changes can make a big difference. Losing 5–7% of body weight and getting at least 150 minutes of physical activity per week (like brisk walking) can significantly lower the risk of progression to type 2 diabetes.
Gestational diabetes develops during pregnancy when hormones from the placenta make it harder for the body to use insulin effectively. While some insulin resistance is normal in pregnancy, in some women it becomes too strong and leads to high blood glucose.Gestational diabetes usually goes away after birth, but it can still affect the health of both mother and baby. Risks include high blood pressure during pregnancy, having a very large baby, or delivery complications. Children exposed to high glucose in the womb are also more likely to develop obesity and type 2 diabetes later in life.Management typically involves lifestyle adjustments and sometimes medication to keep blood glucose levels in a safe range during pregnancy.
(This section is based on guidance from IDF and CDC.2,3)
Symptoms vary by type:
● Type 1 Diabetes
Symptoms can appear suddenly, within just weeks or months, and are often severe. In addition to the common signs, people may also experience nausea, vomiting, or stomach pains.
● Type 2 Diabetes
Symptoms usually develop more slowly—sometimes over several years—and may go unnoticed. In some cases, people may have chest pain, sexual health problems, numbness or tingling in the hands or feet, or wounds that heal slowly.5
● Gestational Diabetes
Most women do not notice symptoms. That’s why doctors recommend screening between 24 and 28 weeks of pregnancy.6
Kidney
damage
Nerve pain,
numbness
& tingling
Vision
Problem
Heart
disease
While each type of diabetes has different causes and symptoms, they all lead to the same result: too much sugar in the blood, which over time can damage the body and cause serious health problems.
Some people may have no symptoms at all, especially in the early stages. An estimated 1 in 3 people living with diabetes remain undiagnosed, and up to half of those diagnosed may not meet their treatment targets .4 Untreated diabetes can damage many major organs, including the heart, blood vessels, nerves, eyes, and kidneys.7
This is why early testing is essential. Being diagnosed early and managing blood sugar well can help prevent serious complications.
For people with diabetes, this system doesn’t work, and although the types of diabetes have different causes, they all end up with too much glucose in the blood which causes a range of complications and health problems.
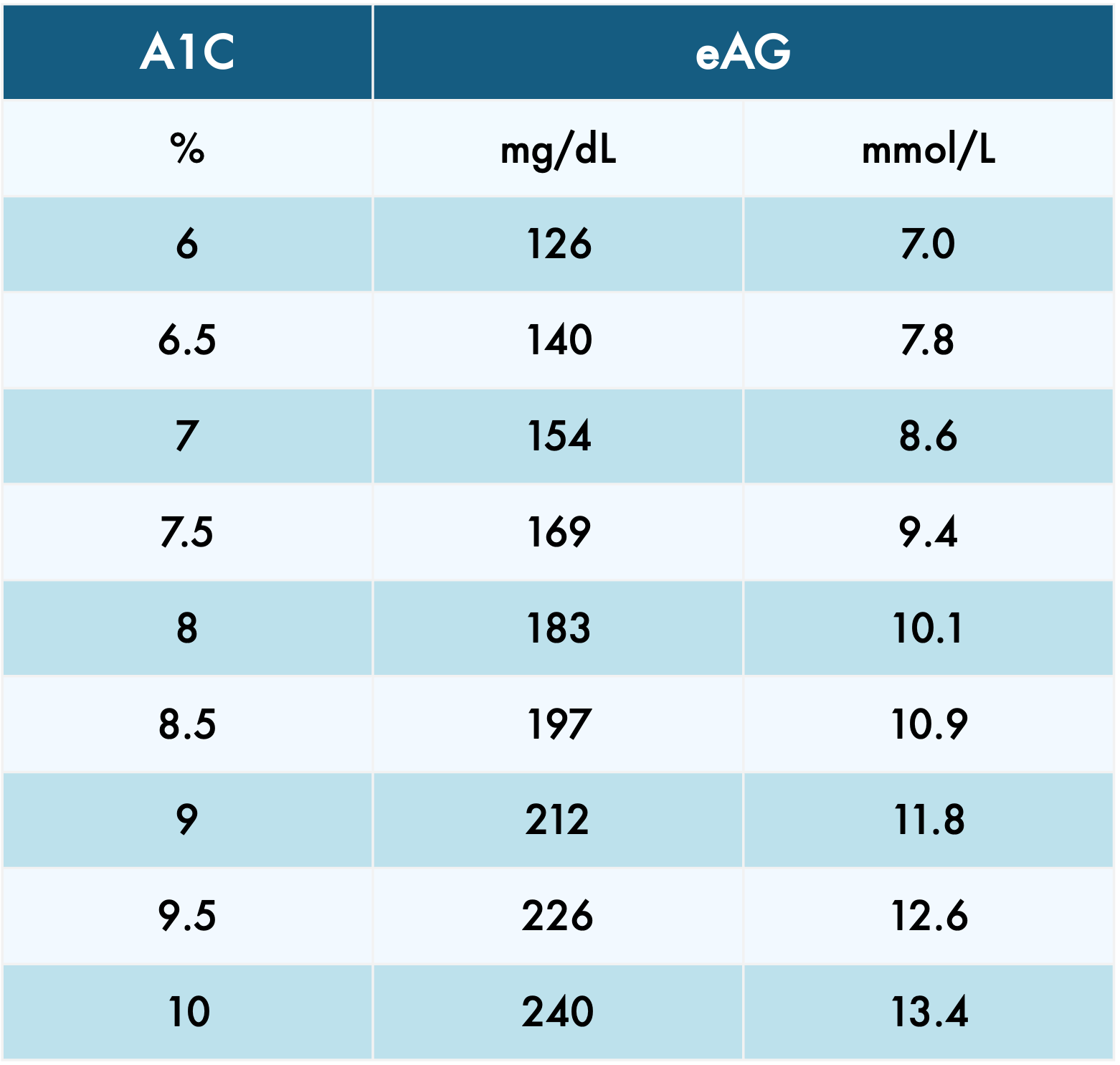
It measures how much glucose is attached to hemoglobin, the protein in red blood cells. Because red blood cells live about three months, the test gives a reliable picture of long-term blood sugar control.
The HbA1c test is widely used to:
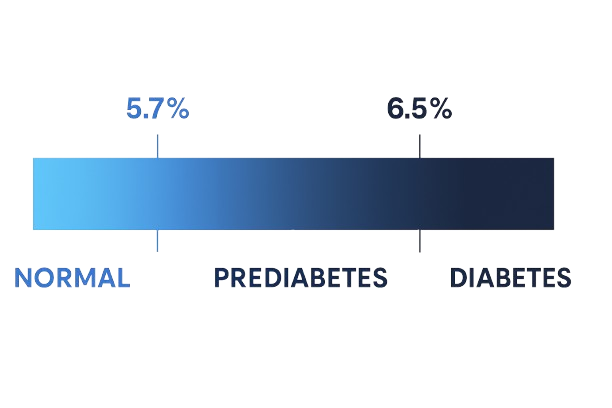
● Detect prediabetes and diagnose diabetes
● Monitor how well treatment is working over time
Your HbA1c goal isn’t the same for everyone. It can depend on your age, overall health, and your doctor’s recommendations. Results are shown as a percentage, which tells you how much glucose has been attached to your red blood cells over the past few months.
The higher the levels, the greater your risk of developing diabetes complications.
● An HbA1c of 6.5% or higher is used as a diagnostic threshold for diabetes.
HbA1c is also reported as eAG (estimated average glucose) which translates the percentage into average daily glucose values—similar to what you see on a glucose meter at home.
● Formula: eAG= (28.7 X HbA1C) – 46.7
● try the ADA calculator here
This section is based on guidance from IDF and ADA.8)
Because everyone’s body and lifestyle are different, it’s important to make it personal, and remember to plan smart, building meal choices, activity, and self-care into your day in a way that keeps your blood sugar balanced over time.
● Healthy Eating9
Choose healthy carbs with fibre – like fruits, vegetables, whole grains, and beans
Pick low-fat dairy and eat oily fish sometimes
Cut back on fatty foods with lots of saturated or trans fats
Be careful with sugar and alcohol
● Physical Activity10
At least 150 minutes of moderate exercise per week
Strength training for muscle and insulin sensitivity
Staying active in daily life (taking stairs, stretching breaks)
● Stress & Mental Health
Practicing stress management (yoga, meditation, breathing exercises)
Seeking support from family, peers, or counselors
Prioritizing sleep and rest
● Monitoring & Regular Check-ups
Keeping track of your blood sugar every day
Following prescribed medication or insulin regimen
Routine visits with healthcare providers
Checking your glucose no longer has to mean pricking your finger every time. With DiaMonTech’s non-invasive glucose monitoring technology, checking your levels can be simple, comfortable, and seamlessly integrated into daily life. Backed by scientific research, our mid-infrared(MIR) photothermal technology has been clinically shown to measure glucose accurately without a single drop of blood.11 We are redefining glucose monitoring—making it effortless, accurate, and accessible for everyone.
1. Centers for Disease Control and Prevention (CDC). Diabetes – Overview. Available at: https://www.cdc.gov/diabetes/about/index.html
2. International Diabetes Federation (IDF). Type 1 Diabetes. Available at: https://idf.org/about-diabetes/types-of-diabetes/type-1-diabetes/
3. Centers for Disease Control and Prevention (CDC). Prediabetes – Prevent type 2 diabetes. Available at: https://www.cdc.gov/diabetes/prevention-type-2/prediabetes-prevent-type-2.html
4. World Health Organization (WHO) Europe. Diabetes Fact Sheet. Available at: https://www.who.int/europe/news-room/fact-sheets/item/diabetes
5. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). Diabetes Overview – Symptoms & Causes. Available at: https://www.niddk.nih.gov/health-information/diabetes/overview/symptoms-causes
6. Centers for Disease Control and Prevention (CDC). Signs and Symptoms of Diabetes. Available at: https://www.cdc.gov/diabetes/signs-symptoms/index.html
7. Diabetes UK. Symptoms of Diabetes. Available at: https://www.diabetes.org.uk/about-diabetes/symptoms
8. American Diabetes Association (ADA). About A1C. Available at: https://diabetes.org/about-diabetes/a1c
9. National Institute for Health and Care Excellence (NICE). Type 2 Diabetes in Adults: Management (NG28). Available at: https://www.nice.org.uk/guidance/ng28/chapter/Recommendations
10. Diabetes Canada. CPG Chapter 10: Nutrition Therapy. Available at: https://guidelines.diabetes.ca/cpg/chapter10
11. Lubinski T, et al. Evaluation of a novel noninvasive blood glucose monitor based on mid-infrared quantum cascade laser technology and photothermal detection. Journal of Diabetes Science and Technology. 2020; 14(6):1046–1051. Available at: https://doi.org/10.1177/1932296820936634
12. Hermanns N, et al. Coordination of glucose monitoring, self-care behaviour and mental health. Diabetologia. 2022. Available at: https://link.springer.com/article/10.1007/s00125-018-4729-5